In my more decades of life than I care to admit, 2025 has gotten off to the roughest start ever! It seems like everything – cars, major appliances and yes, even bodies – is either falling apart, or in need of extensive repairs. But of all these, the one that impacted my life the most began on February 3rd. Yes, I remember the exact date. I noticed a minor ache in my hip during my daily power walk. Nothing unusual, just stretch it out and keep going the same as always, right? Wrong. This time, the ache blew up. By the following evening, I was barely able to walk. After a trip to urgent care, a spine specialist (for what turned out to be a false lead), and eventually a late-night ride to the emergency room, I was admitted to the hospital in excruciating pain. That was only the beginning. It took a total of three separate admissions before I finally went home for the last time, hobbling on a walker.
Things have slowly improved for me since then. And as you might expect, the healthcare I received during that time has left me with many lasting impressions. Yet the thing I feel most compelled to write about is the food I was served during my three stays in the hospital. As a person with dietary restrictions, accommodating my nutritional needs turned out to be a far more complicated, stressful and frustrating experience than I would have expected from a hospital, of all places.
My first admission was via the emergency department. They wheeled me out of the ER and up to my room in the middle of the night. As the staff connected me to monitoring equipment, medications and my dietary restrictions were discussed. I explained to the nurse that I was both vegan and gluten-free, and had been so for several decades; i.e., this was not a fad diet for me. I also noted that I was allergic to oranges; a fact she was already aware of, as it was in my medical record.
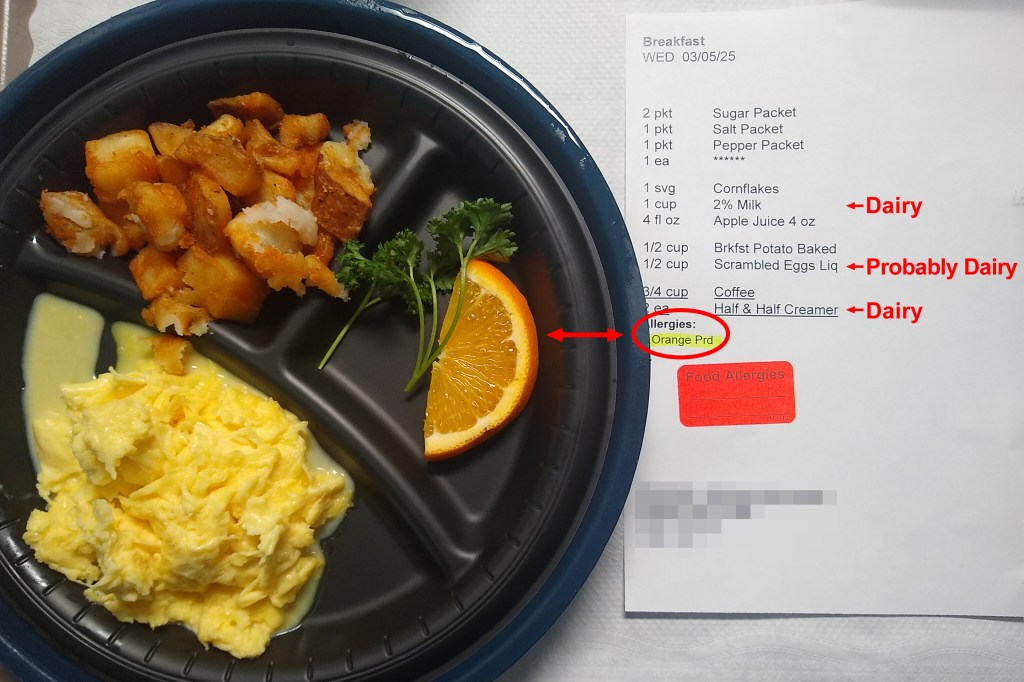
Breakfast arrived: juice, milk, eggs, toast and meat. All pretty standard fare, except for one problem: it contained absolutely nothing a gluten-free vegan could consume, aside from the juice. Thankfully my husband was there, and he spoke with the nurse. She affirmed that she had documented our earlier discussion in my electronic medical record, and requested a nutrition consult. Later that day, the nutrition supervisor paid me a visit. She seemed receptive to my nutritional needs. Throughout the remainder of my first hospital stay, my meals were built around various store-bought Amy’s gluten free and vegan products. I later learned that this seemingly simple accommodation was apparently a bit of a challenge for the hospital’s dietary department, as they are locked into a predefined set of choices through a handful of institutional suppliers. With little provision for specialty diets, and no allowance for off-menu customization, a simple trip to the local supermarket for you and me was a major procedural hurdle for them. I imagine the supervisor herself went to the store and purchased the meals: tofu burritos for breakfast, vegetable burgers for lunch and either vegetable loaf, vegetable lasagna or enchiladas for dinner. I was also provided more than my share of fruit, including oranges on several occasions, despite the allergy alert in my medical record (See Figure 1). Yet despite these hiccups, if my first stay in the hospital had been the end of my nutritional experience there, I would have left feeling that their nutrition department had at least made a concerted effort to accommodate my needs, albeit with a fair amount of hidden sodium (read on). Unfortunately, the disappointment and frustration that followed was unimaginable beyond belief.
Figure 1: Hospital Breakfast Tray
I was readmitted to the hospital twice. From a dietary standpoint, you would have thought I was sent to an entirely different hospital surrounded by cattle farms in the middle of Kansas. Despite the fact that less than a week passed since my initial admission, and the whiteboard in my hospital room indicated that I followed a gluten-free vegan diet, compliant food was nowhere to be found (See Figure 2). They couldn’t even muster up gluten-free vegan bread! Beyond a few half-hearted efforts, it was as if they had effectively given up.
Figure 2: In-Room Hospital Patient Information Board

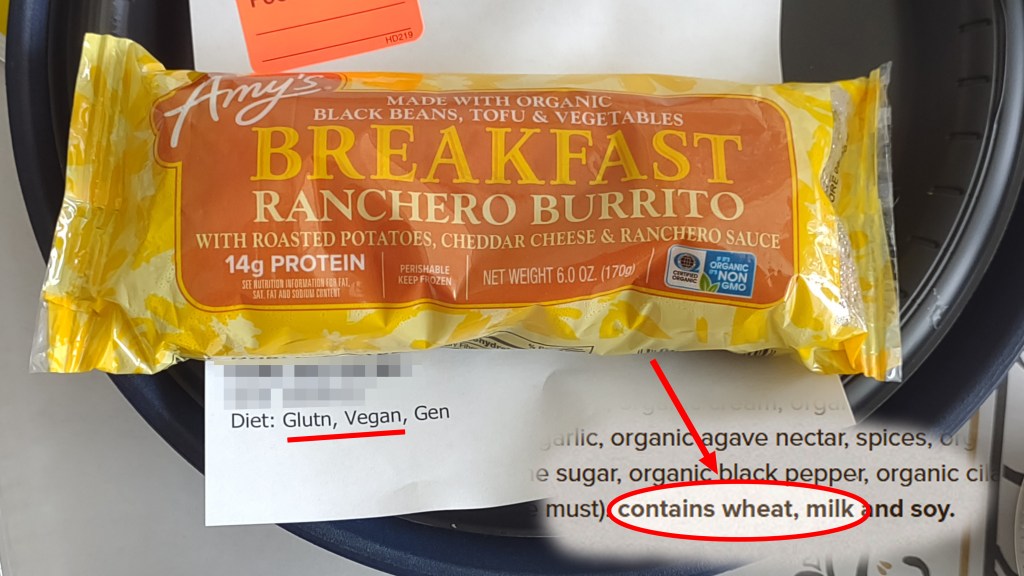
For example, although someone once again made an attempt to purchase Amy’s burritos (a non-hospital food) for my consumption, they selected varieties containing gluten and dairy, rendering them incompatible for me, (see Figure 3). I can only surmise that whoever was sent out to purchase them mistakenly assumed that all Amy’s products are vegan and gluten-free (they are not). Expecting someone from a hospital’s nutrition department to actually read a nutrition label was simply too much to ask. Another possible explanation: the store had no gluten-free, vegan Amy’s products in stock on the day they visited (a common occurrence with allergen-friendly items), so they simply grabbed what they could, rather than spend time traveling to another store with potentially the same results. On our own trips to the supermarket, or even specialty chains like Sprouts and Whole Foods, we routinely experience difficulty in finding these products on a reliable basis. Yes, the freezer case will be packed with Amy’s products, just none that are gluten-free and vegan. Also, many plant-based and allergen-friendly products are loaded with sodium and fat, and are not necessarily as healthy as people may assume. Lastly, I should point out that it seems as if they developed a case of Amy’s tunnel vision. There are other options, but Amy’s was the quick and easy go-to fix. Except when it wasn’t in stock, something the dietary department seemed absolutely unprepared for.
Figure 3: Label Reading Failure: Amy’s Breakfast Burrito Containing Dairy and Gluten
What was so mindboggling was that I was in a moderately large Southern California hospital in the middle of progressive La-La Land. California is the state with the largest number of vegan restaurants! Moreover, I was in a hospital in Los Angeles (LA) County, home to roughly 30 exclusively vegan restaurants. Given the popularity of veganism here, one would expect that the local hospitals would be adept at accommodating a vegan diet. Now you may be thinking, a vegan diet is one thing, but a diet that is both vegan and gluten-free is simply insurmountable. After all, the hospital seems to have thought so. Thankfully however, this is not the case! There are at least two dozen popular gluten-free restaurants in LA County alone, many of which offer an extensive vegan menu.
So, why was this moderately large Southern California hospital so ill-equipped to deal with a fairly common (for LA) diet? It appears their nutrition department, like LA’s public education system is as clunky as machinery from the Industrial Revolution, with a gluten-free vegan diet representing the modern-day equivalent of a proverbial monkey wrench in the gears, or as the British say, “a spanner in the works.”
The hospital gave the appearance they cared by having a representative from the nutrition department speak to me daily, either by phone or in person in my room. Turns out those discussions were window dressing, as what actually showed up at mealtime rarely resembled anything we had discussed. Worse, during my concluding hospitalization, the dietary representative finally gave up and literally said, “I have nothing for you” after I declined her offer for a meat burger.
Do you remember the 1970’s Burger King jingle?
Hold the pickle, hold the lettuce
Special orders don’t upset us
All we ask is that you let us serve it your way
Have it your way, have it your way
Have it your way, at Burger King
As someone who worked at Burger King as a teenager many decades ago, and who, as a vegetarian then, was ironically able to muster together food to eat there, the jingle popped back into my mind. Only this time, I modified it for this hospital:
Vegan, gluten-free? Don’t ask us
Special diets, they upset us
All we ask is that you let us serve it our way
Have it our way, only our way
Have it our way, during your stay
Since items such as rice-based dishes, vegan meat, legumes (including lentils and beans) or even just a salad topped with vegetables and tofu were not an option, I had to rely on my husband to bring food and tea from home. In the midst of all this, I was happy to discover that chamomile tea, with its zero-caffeine content, was a regular item on the hospital’s menu. And yet, believe it or not, I frequently received coffee instead. The degree of dysfunction spread to even their own regular menu items! You may ask: if so, wasn’t I in the same boat as all the other patients? Why was my case so unique? Because if things are that problematic in general, they are even more broken for a restricted diet. What was so frustrating was the apparent lack of concern for my nutritional needs. I was in a hospital for G-d’s sake! Lunches often consisted solely of a few condiment-sized containers filled with fruit. Yes, fruit and nothing else. Even the nurse’s aides bringing me my food tray would apologize as they sat it down on my table. I was told on more than one occasion, it “may be best to Uber in food.” Honestly? Given what I (and my insurance company) was likely charged for meals, along with the fact that my family is not a member of California’s wealthy resident’s club, ordering out was simply not an option. I am fully aware of the higher cost of allergen-friendly restaurant fare in Los Angeles County. It is the primary reason my family does not often eat out.
Figure 4: Fruit, Fruit and More Fruit.

So, you may be wondering what I actually ate during my second and third hospitalizations. A typical day consisted primarily of food items brought from home, plus whatever the hospital provided that I could actually consume (i.e., mainly small containers of melon fruit). This meant that food brought in from home could not require refrigeration or freezing, as it was kept in bags in my room. As a result, breakfast often consisted of home-brought items such as gluten-free and vegan cereal with plant-based milk, and gluten-free bread with almond butter and banana for lunch. Dinner? You guessed it, whatever my husband prepared at home and brought to the hospital.
My husband often spent the night sleeping on a fold-down sofa bed in the hospital room. As a result, prior to leaving for work each morning, he would go down to the cafeteria and purchase chamomile tea and plant based-milk. Yes, we were able to purchase both of these items in the hospital’s cafeteria, but were unable to order plant-based milk from the dietary department, and it was hit or miss on whether I received chamomile tea or not. Not to mention the periodic oranges that appeared on my hospital trays.
Figure 5: When It’s Not on the Inpatient Menu: Nutrition Hacks from the Hospital Cafeteria


The nurses and aides repeatedly apologized. They kept telling me “we contacted dietary.” But, aside from that, what else could they really do? Leave the hospital and shop for meals for me themselves? If push came to shove, I truly believe some of them would have. However, they are obviously not part of the food service mechanism that is actually responsible for the nutritional needs of its patients.
A hospital is rightfully viewed as a place where people go to be healed. Little attention is paid to whether or not the facility’s nutrition department will be able to accommodate someone’s dietary needs. One simply assumes that it will. I certainly did. Unfortunately, my three recent stays in the hospital are testament that this is not always the case, even in geographical areas where alternative diets and healthier lifestyles are widely publicized, if not celebrated.
The failure of any hospital’s nutrition department to meet the needs of ALL of its patients can result in a multitude of consequences that may delay the healing process: malnutrition, imbalances in electrolytes and other essential elements (such as iron), an increase in the severity of other co-occurring conditions (such as celiac disease), or allergic reactions (to allergens such as dairy and oranges), to name a few. Had I been left with no recourse but the meals the hospital offered, I would have been forced to turn away almost everything. Not out of stubbornness, nor by choice, nor from some perverse desire to be a “difficult patient,” but because consuming most of that food would literally have made me more ill. By that admittedly dismal standard, inadequate nutrition would be the less damaging alternative. People who can tolerate a mainstream diet are often somewhat baffled and annoyed by those of us who cannot. While this can be awkward and inconvenient around the communal table, it’s far more serious in a hospital setting. I do not enjoy making life more complicated for those entrusted with providing for my care, but I have to advocate for what I know to be in my own best interests. And quite frankly, sometimes that means you just have to be a pain in the ass. It’s one of the only ways to push back against potentially detrimental, one-size-fits-all service from an enormous enterprise that, even when well-intentioned, just wants to keep rolling along on its own momentum.
To end this piece on a positive note, I must mention that I had some stellar nurses who, as described above, probably would have gone to one of the local grocers and purchased food for me themselves, if my husband was unable to be at the hospital on a daily basis. However, all things being equal (nursing staff, physicians, laboratory and pharmacy), should I need hospitalization in the future, I would elect to receive care at another LA-based hospital where I was not left to fend for myself when it came to meeting my nutritional needs. It is a burden that no one should have to contend with during the already stressful situation of being hospitalized.
